Radiation Therapy
What is radiation therapy?
One third of cancer children are treated by radiation therapy in their initial management, which represents 700 pediatric radiations performed per year in France within specialized accredited centres according to the National Cancer Institute (INCa) recommendations. The Centre Léon Bérard is one of these centres and as such, manages children from the Auvergne Rhône-Alpes Region (apart from children managed in Grenoble where this management is performed as well). Moreover, the Centre léon Bérard radiation therapy unit is a referral centre for some particular techniques on pediatric radiation therapy (radiation under anesthetic, curie-therapy, stereotaxic…) and manages as such children outside the region. All radiation techniques are available on the site of Lyon (Intensity-Modulated Radiation Therapy, tomotherapy, VMAT, cyberknife, curie therapy…) apart from proton therapy for which collaboration with the Orsay and Nice centres will be implemented shortly.
Treatment protocols follow the French Society of Child Cancers (SFCE) or prospective French and European protocols. Technical or ballistic choice can be discussed during bi-monthly national web-conferences on pediatric radiation therapy techniques. Radiation therapy consists in ionizing radiations (usually photons, electrons or protons more rarely) on a specific tumour area to kill cancer cells.
Depuis que je suis malade,
je me pose beaucoup de questions :
qu’est-ce que je peux faire ?Trouver une réponse aux questions
de vos enfants !
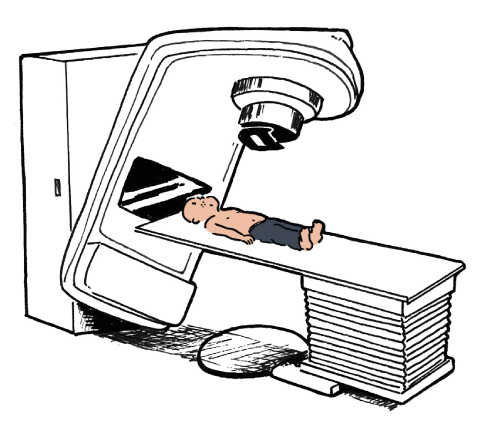
How does the treatment take place?
- Consultation with the radiotherapist
The radiation therapy decision, like all strategic treatment decisions, is discussed within an inter-regional Multidisciplinary Tumour Board, to which the child referent pediatric oncologist participates. The implementation of the radiation therapy requires a specialized consultation with a radiotherapist, with skills in pediatrics, who will meet the child and the parents to explain the expected benefic outcomes and the possible side effects.
- Screening: dosimetry scan
The first stage of the treatment is a “location” stage, also called “dosimetry scan”. It is performed in the radiation therapy department, in the same position as the treatment position. Usually, there is no injection, but it may sometimes be necessary and it will be explained by the radiotherapist during the consultation. A MRI called “merge MRI” is sometimes required to optimize the tumour delineation (head and neck tumours and spine). All sessions must be performed in the same position so as to give the patient an optimal treatment. That requires the child to be calm and laid most of the time in an immobilisation device (ball mattress, mask…). All procedures regarding contention, scan and session are HARMLESS. They can be annoying because the child must be kept immobilized but they are never painful. Relaxing techniques (musical ritual, hypnosis…) can be offered if required.
- Radiation therapy sessions
They usually take place from Monday to Friday, except on bank holidays. Sessions can be set up either in the morning or in the afternoon. They last from 10 to 30 minutes according to the techniques. They are harmless. You can eat or drink before the session. The immobilization device is placed again before each treatment and for the time the session lasts. One parent will be authorized to take the child to the treatment room but he will then have to wait in the waiting room during the session. It is not allowed for anybody else but the patient to stay in the treatment room. The radiation operator can keep a visual and hearing link with the child thanks to a camera and a microphone. It is possible to listen to some music or to some stories recorded on CDs during the session upon the child request. MP3s should not be taken inside the radiation room for they could be damaged by the radiation.
- Following the sessions
A child who received radiations is not “irradiant”, he can safely be in contact with his family as well as with young children or pregnant women. Education is possible upon agreement of the referent pediatric oncologist, who can sometimes make adjustments according to the radiation therapy and the concomitant treatments of chemotherapy: classical school, most often part time, IHOPE School, school at home…avoid in any case a sun exposure on the irradiated field (restrictive exposure especially during the hottest hours of the day, high sunscreen cream, covering clothes…). The food diet is usually normal during radiation therapy unless chemotherapy requires a special diet. It may be necessary to control blood biology (blood test) if radiation therapy was performed on large volumes, this will be discussed with the radiotherapist during the consultation
Who will look after my child during this treatment?
The pediatric radiotherapist is in charge of the treatment. He meets the child during the initial examination and on weekly consultation during the radiation therapy treatment. In his absence he may be substitute by one of his colleagues or a resident radiotherapist. During each session the child will be managed by operators who will make sure your child is in the right position, that an imaging control which may have to be done before the session is performed and that the treatment session is performed.
The link with the referent oncologist will be kept especially if chemotherapy has to be performed during the radiation therapy.
How will this treatment impact the cancer of my child?
Radiation therapy is a local treatment. Its action is thus limited to the irradiated field, with no general effect. The main aim of irradiation is to kill cancer cells by stopping their division by destroying the cell core (DNA damaged).
At the IHOPE Everything is set up for the children comfort and well-being..
Espaces de détente
EN SAVOIR PLUS
Activités et loisirs
EN SAVOIR PLUS
Confort et bien-être
EN SAVOIR PLUS
A quels effets secondaires peut-on s’attendre
lorsque mon enfant sera confronté à la radiothérapie ?
Les effets secondaires de la radiothérapie sont très variables en fonction des doses délivrées, du site irradié, de l’âge de l’enfant principalement. Il n’est pas possible de les détailler simplement ici. Le radiothérapeute expliquera lors de la consultation initiale et si besoin lors du suivi ces effets secondaires et leur éventuelle prise en charge. Globalement, on distingue :
- Les effets secondaires aigus de l’irradiation qui surviennent pendant ou dans les quelques semaines suivant la radiothérapie ; ils sont habituellement réversibles. Par exemple, en cas d’irradiation du cuir chevelu, une perte de cheveux est attendue ; en cas d’irradiation de la peau, l’équivalent d’un « coupe de soleil » habituellement modéré peut apparaitre , etc…
- Les effets secondaires tardifs de l’irradiation qui peuvent apparaitre dans les mois ou années qui suivent la radiothérapie ; ils ne sont pas toujours réversibles et seront expliqués au cas par cas par le radiothérapeute, en fonction du site tumoral irradié.
Cas particulier des enfants très jeunes
Dans le cas d’un enfant jeune (habituellement moins de 4-5 ans), une anesthésie générale (sédation profonde) pourra être nécessaire afin d’assurer le repositionnement correct de l’enfant à chaque séance. Une consultation avec les médecins anesthésistes sera alors nécessaire au préalable pour que les parents reçoivent les explications sur la prise en charge de leur enfant.
La radiothérapie offre des techniques complexes et innovantes. Pour plus de renseignements, nous vous invitons la lire la page consacrée à la radiothérapie dans le site internet du Centre Léon Bérard.